Abstract
The BTK-inhibitor ibrutinib is the first FDA approved therapy for Waldenström macroglobulinemia (WM) and produces overall response rates >90% and long-term disease control in both treatment naïve and previously treated patients. Despite the remarkable efficacy of ibrutinib, dose reduction is often required for intolerance. In this study, we analyzed those patients requiring a dose reduction and evaluated the time to dose reduction, the symptoms leading to dose reduction, the rate of improvement in symptoms after dose reduction, and the hematologic response at 12 months after dose reduction.
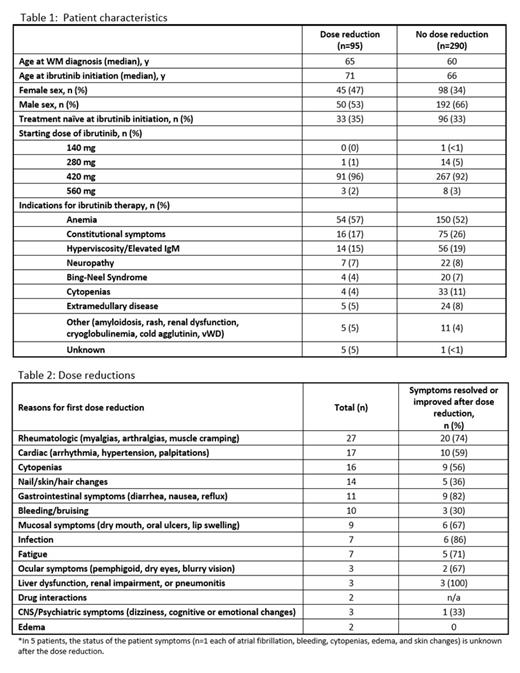
385 patients received treatment with ibrutinib in our clinic from May 2012 through October 2020. Their baseline characteristics are shown in Table 1. Starting dose for these patients was 560 mg (n=11); 420 mg (n=358); 280 (n=15); 140 mg (n=1). Approximately 1/3 of all patients were treatment naïve at the time ibrutinib was initiated. Anemia, constitutional symptoms, and symptomatic hyperviscosity (or risk of hyperviscosity) were the most common reasons for treatment initiation. Reasons for dose reduction are shown in Table 2. Ninety-five patients (25%) required at least one dose reduction of ibrutinib. Twenty-three patients (6%) required a second dose reduction. Of the patients requiring dose reductions, 1 patient started at 280 mg and reduced to 140 mg, 91 patients started ibrutinib at 420 mg (1 patient ultimately had dose reduction to 70 mg, 22 patients to 140 mg, and 68 patients to 280 mg), and three patients started ibrutinib at 560 mg in the setting of Bing-Neel syndrome (2 patients had dose reduction to 420 mg and 1 patient to 280 mg).
Patients requiring a dose reduction had a median age of 71 years (range, 46-96) at the time of ibrutinib initiation versus 66 years (range, 40-93) for those not requiring a dose reduction (p<0.001). Forty-five patients (47%) of patients requiring dose reduction were female versus 98 (34%) not requiring dose reduction (p=0.017).
Median time to first dose reduction was 7.3 months (range, 0.5-75) and median time to second dose reduction from initiation of ibrutinib was 23 months (range, 3-75). Of the 95 patients requiring a dose reduction, 40 patients (42% of all patients with dose reductions) had improvement in at least 1 of the medication side effects after the initial dose reduction. Twenty-two patients (23%) had complete resolution of adverse effects. Twenty-six patients (27%) had no change in symptoms and 10 of these patients required an additional dose reduction. After the second dose reduction, 5 patients had improvement or resolution in symptoms. Two patients had no adverse effects prior to dose reduction and medication was reduced simply due to drug interaction.
Of the 48 patients with 1-year hematologic follow-up data available, 10 patients (21%) had improvement in hematologic response and 35 patients (73%) maintained their hematologic response despite dose reduction. Three patients (6%) had worsening of hematologic response after dose reduction.
In conclusion, one quarter of WM patients in this series on ibrutinib required a dose reduction due to development of intolerable medication side effects. In the majority of these patients, adverse effects improved or resolved with dose reduction. Importantly, hematologic response remained stable or improved in most patients despite dose reduction.
Treon: BeiGene: Consultancy, Research Funding; Eli Lily: Research Funding; Abbvie/Pharmacyclics: Consultancy, Research Funding. Castillo: Abbvie: Consultancy, Research Funding; BeiGene: Consultancy, Research Funding; Pharmacyclics: Consultancy, Research Funding; Janssen: Consultancy; Roche: Consultancy; TG Therapeutics: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal